Navigating the world of skilled nursing facilities (SNFs) can feel like traversing a complex maze, especially when it comes to documentation. With the Patient-Driven Payment Model (PDPM) now the standard, precise and comprehensive nursing documentation is more crucial than ever. It’s not just about ticking boxes; it’s about painting a clear picture of the patient’s needs, progress, and the skilled care they receive. This ensures accurate reimbursement, but more importantly, it facilitates optimal patient outcomes. Let’s face it, disorganized or incomplete documentation can lead to denied claims, compliance issues, and potentially, compromised patient care. So, where do you even begin to streamline this essential process?
Think of a nursing documentation template for PDPM as your roadmap through that maze. It’s a standardized framework designed to guide nurses in capturing all the necessary information required for accurate PDPM coding and billing. Essentially, it helps ensure that the facility gets reimbursed appropriately for the level of care they’re providing. The right template prompts thorough assessments, tracks changes in patient condition, and outlines the specific interventions implemented. This isn’t just about financial security; it’s about enabling facilities to continue delivering high-quality care to their residents.
In this article, we’ll explore the key elements of an effective nursing documentation template for PDPM, highlighting the importance of each section and offering practical tips for implementation. We’ll delve into the ‘why’ behind the ‘what,’ helping you understand how accurate documentation translates into better patient care and improved financial stability for your facility. We will also look at how a well-designed template can reduce the burden on your nursing staff, freeing them up to focus on what matters most: providing compassionate and effective care.
Essential Elements of a Robust Nursing Documentation Template for PDPM
Crafting an effective nursing documentation template for PDPM isn’t a one-size-fits-all endeavor. It requires careful consideration of the specific needs of your facility and the patient population you serve. However, certain key elements are fundamental to any successful template. These elements ensure that all relevant information is captured accurately and efficiently, supporting both clinical decision-making and accurate reimbursement under PDPM. Let’s explore these elements in detail.
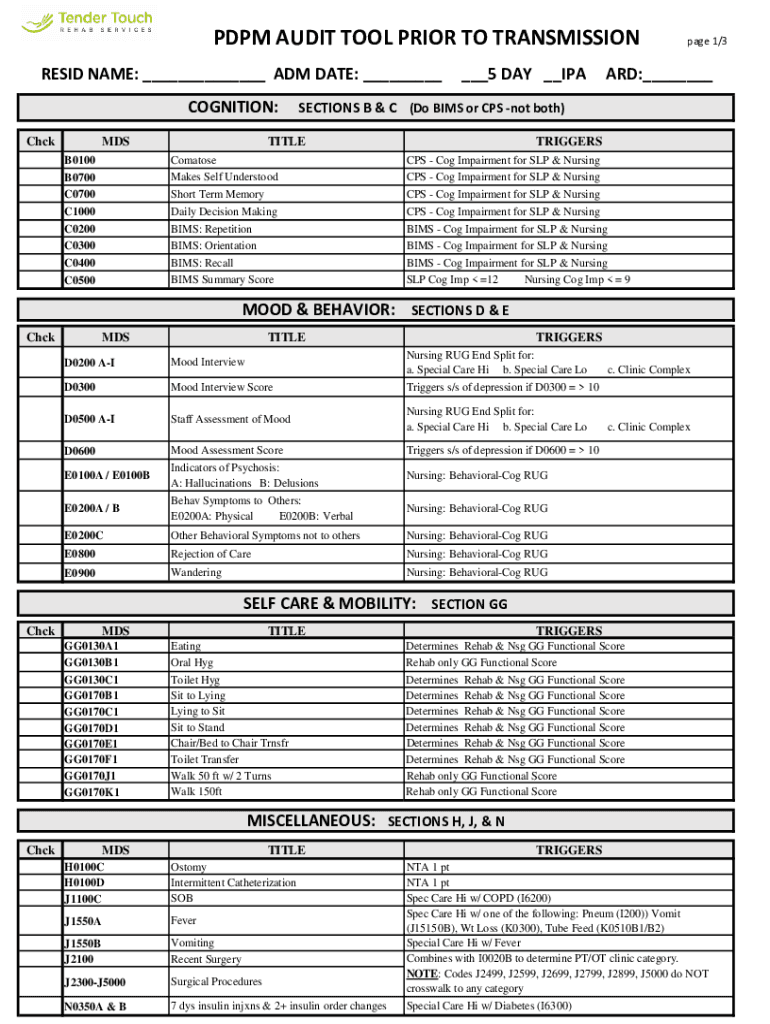
First and foremost, the template must include comprehensive sections for patient assessment. This goes beyond basic vital signs and general observations. It necessitates detailed evaluations of the patient’s functional status, including mobility, cognition, communication abilities, and swallowing function. These assessments are critical for determining the appropriate PDPM classification and ensuring that the care plan accurately reflects the patient’s needs. Standardized assessment tools, such as the Minimum Data Set (MDS), should be integrated into the template to ensure consistency and accuracy.
The template should also feature dedicated sections for documenting the skilled nursing services provided. This includes detailed descriptions of wound care, medication administration, respiratory treatments, and any other interventions requiring the expertise of a registered nurse or licensed practical nurse. Clear and concise documentation of these services is essential for demonstrating the need for skilled care and justifying the associated reimbursement. Furthermore, the documentation should include the frequency, duration, and intensity of these services, as well as the patient’s response to treatment.
Another crucial element is the inclusion of a section for documenting changes in the patient’s condition. PDPM is a dynamic payment model that adjusts based on the patient’s changing needs. Therefore, it’s essential to track any significant changes in functional status, cognitive abilities, or medical conditions. These changes should be documented promptly and thoroughly, as they may trigger a reassessment and a potential adjustment to the PDPM classification. This section should also include documentation of any adverse events, such as falls or medication errors, and the interventions implemented in response.
Finally, the template should facilitate interdisciplinary communication. This means providing a space for nurses to document their observations, concerns, and recommendations, as well as a mechanism for sharing this information with other members of the care team, such as physicians, therapists, and social workers. Effective communication is essential for ensuring coordinated and holistic care. This can be achieved through progress notes, care conferences, and electronic health record (EHR) integration. The goal is to create a seamless flow of information that supports optimal patient outcomes and accurate PDPM coding.
Tips for Optimizing Your Template
Beyond the core elements, consider these tips to make your nursing documentation template for PDPM truly effective:
* Make it user-friendly: Design the template to be intuitive and easy to navigate, minimizing the time nurses spend on documentation.
* Incorporate drop-down menus and checklists: These tools can streamline the documentation process and reduce the risk of errors.
* Provide clear instructions and training: Ensure that all nursing staff are thoroughly trained on how to use the template and understand the importance of accurate documentation.
* Regularly review and update the template: As PDPM guidelines evolve, be prepared to adapt your template to ensure compliance and accuracy.
Implementing and Maintaining Your Nursing Documentation Template for PDPM
Developing a solid nursing documentation template for PDPM is only half the battle. The real challenge lies in implementing it effectively and ensuring that it remains a valuable tool for your nursing staff. A successful implementation requires careful planning, consistent training, and ongoing monitoring. Let’s explore the key steps involved in this process.
First, gain buy-in from your nursing staff. Explain the benefits of the new template, not just in terms of PDPM compliance but also in terms of improved patient care and reduced administrative burden. Emphasize how the template can help them streamline their documentation process and focus more on direct patient care. Address any concerns or resistance they may have by providing clear and concise answers to their questions. Active involvement of the nursing team during the design phase, if possible, can greatly assist with gaining buy-in.
Next, provide comprehensive training on the new template. This training should cover all aspects of the template, including how to navigate it, how to complete each section accurately, and how to use any associated electronic tools. Hands-on practice is essential to ensure that nurses feel comfortable and confident using the template. Consider offering ongoing support and refresher training to reinforce the key concepts and address any questions that arise over time.
Regularly monitor the use of the template to ensure that it is being implemented correctly. This can involve reviewing a sample of completed templates to identify any areas where improvement is needed. Provide feedback to nurses on their documentation practices and offer additional training or support as needed. Consider using audits to identify trends and areas for improvement. This will help to ensure the integrity and accuracy of the data being collected.
Integrate the template into your facility’s electronic health record (EHR) system, if possible. This will streamline the documentation process and facilitate interdisciplinary communication. Ensure that the template is easily accessible to all members of the care team and that it is updated whenever changes are made. A well-integrated EHR can significantly reduce the risk of errors and improve the efficiency of the documentation process. Electronic integration can reduce the number of hours spent in documentation.
Finally, stay informed about changes to PDPM guidelines. As the Centers for Medicare & Medicaid Services (CMS) updates its policies and procedures, be prepared to adapt your template accordingly. Regularly review the CMS website and other relevant resources to stay abreast of the latest developments. This will help you to ensure that your facility remains in compliance with PDPM regulations and continues to receive appropriate reimbursement for the care you provide. A nursing documentation template for pdpm needs to be consistently updated to accurately capture all information required for accurate PDPM coding and billing.
Adopting an organized system enables facilities to maintain comprehensive patient information. This structured approach facilitates effective communication among healthcare professionals, fostering collaboration and ensuring continuity of care, which, in turn, enhances patient outcomes and reduces the potential for errors.
By focusing on meticulous record-keeping, facilities not only demonstrate regulatory compliance but also enhance their operational efficiency and financial stability. This proactive approach ensures that your facility remains a trusted provider of high-quality care within the ever-evolving landscape of long-term healthcare.



