Wound care is a critical aspect of healthcare, requiring meticulous attention to detail and accurate record-keeping. Imagine a nurse, pressed for time, needing to quickly and effectively assess a patient’s wound. A well-designed wound assessment documentation template becomes an indispensable tool, guiding them through the necessary observations and ensuring consistent data collection. This isn’t just about ticking boxes; it’s about painting a clear picture of the wound’s characteristics and tracking its progress over time, enabling informed decisions regarding treatment and management.
Think of a wound assessment documentation template as a standardized roadmap for evaluating and documenting various aspects of a wound. It’s more than just a form; it’s a framework that helps healthcare professionals systematically gather information about the wound’s appearance, size, surrounding tissue, pain levels, and any signs of infection. Using such a template improves communication among healthcare providers, ensuring everyone is on the same page regarding the patient’s condition and treatment plan. It also helps in monitoring the effectiveness of interventions and making necessary adjustments along the way.
The beauty of a good wound assessment documentation template lies in its ability to streamline the assessment process while capturing comprehensive details. In the hustle and bustle of a busy healthcare setting, having a structured approach ensures that nothing is overlooked. From the initial assessment to ongoing monitoring, a consistent template promotes accuracy, reduces errors, and ultimately contributes to better patient outcomes. It’s about empowering healthcare professionals with the right tools to deliver the best possible care.
Why Accurate Wound Assessment Documentation Matters
Accurate wound assessment documentation is the cornerstone of effective wound management. Imagine trying to navigate a complex medical case without a clear and detailed record of the patient’s condition. Without accurate documentation, healthcare providers risk making decisions based on incomplete or inaccurate information, potentially leading to delayed healing, complications, or even adverse events. This is why a standardized approach using a wound assessment documentation template is so crucial.
Think about the legal implications as well. In today’s healthcare environment, detailed documentation is essential for protecting both patients and providers. A comprehensive record of wound assessments, treatment plans, and patient responses serves as a valuable reference in case of audits, legal challenges, or quality improvement initiatives. Clear and concise documentation demonstrates that the standard of care was met and that appropriate interventions were implemented. This provides a sense of security and accountability for everyone involved in the patient’s care.
Moreover, consistent documentation facilitates effective communication and collaboration among healthcare team members. Nurses, physicians, therapists, and other professionals can easily access and review the patient’s wound history, enabling them to make informed decisions and provide coordinated care. This is particularly important in complex cases that require multidisciplinary expertise. A shared understanding of the wound’s characteristics and progress ensures that everyone is working towards the same goals.
Beyond immediate patient care, accurate wound assessment data contributes to valuable research and quality improvement efforts. By analyzing aggregated wound data, healthcare organizations can identify trends, evaluate the effectiveness of different treatment modalities, and develop evidence-based guidelines for wound management. This continuous cycle of data collection, analysis, and implementation leads to improved outcomes and better overall care for patients with wounds.
Ultimately, accurate wound assessment documentation is about putting the patient at the center of care. By meticulously recording wound characteristics, pain levels, and other relevant information, healthcare providers gain a deeper understanding of the patient’s experience and can tailor treatment plans to meet their individual needs. This patient-centered approach not only promotes healing but also enhances the patient’s overall well-being and quality of life. The wound assessment documentation template supports this goal.
Key Components of an Effective Wound Assessment Template
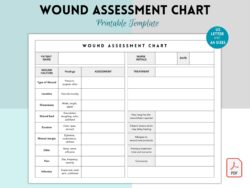
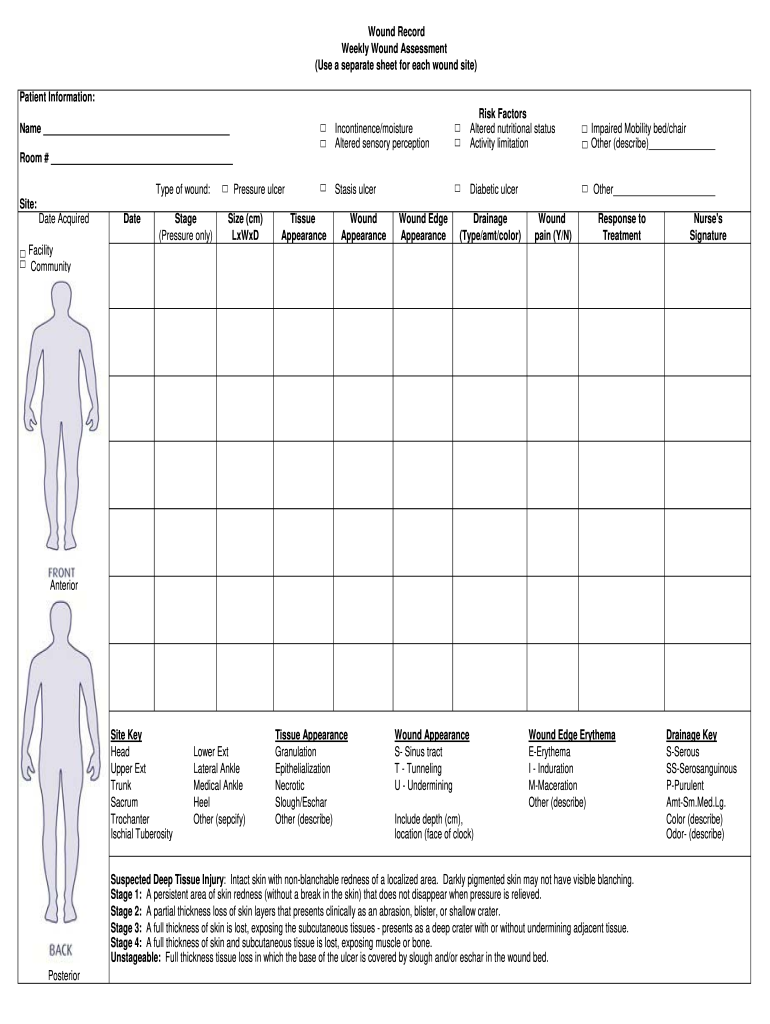
A well-designed wound assessment template incorporates several key components to ensure comprehensive data collection. This isn’t just about filling out a form; it’s about creating a tool that guides healthcare professionals through a systematic and thorough evaluation of the wound. Let’s explore some of the essential elements that should be included in every effective wound assessment documentation template.
First and foremost, the template should include fields for basic patient information, such as name, date of birth, medical record number, and admitting diagnosis. This helps to accurately identify the patient and track their wound care history. Additionally, the template should include the date and time of the assessment, as well as the name and credentials of the healthcare professional performing the assessment. This ensures accountability and provides a clear timeline of wound-related events.
Next, the template should capture detailed information about the wound itself. This includes the location of the wound, its size (length, width, and depth), shape, and any undermining or tunneling. It’s also important to document the type of tissue present in the wound bed, such as granulation tissue, slough, or eschar. The color and odor of the wound should also be noted, as these can be indicators of infection. Describing the periwound skin, which is the skin surrounding the wound, is also crucial. Look for signs of maceration, erythema, or edema.
Pain assessment is another essential component of a comprehensive wound assessment template. Patients should be asked to rate their pain level using a standardized scale, such as a numeric rating scale or a visual analog scale. The type, frequency, and duration of pain should also be documented. Understanding the patient’s pain experience is crucial for developing effective pain management strategies.
Finally, the template should include sections for documenting the treatment plan, any interventions performed, and the patient’s response to treatment. This includes the type of dressing used, the frequency of dressing changes, and any topical medications applied. It’s also important to document any complications that arise, such as infection or bleeding, and the steps taken to address them. Regular reassessments are key, and the template should allow for tracking changes in the wound over time. Using a wound assessment documentation template ensures consistent and thorough data collection, leading to better patient outcomes.
Using a structured template for wound assessment ensures that no crucial information is missed, promotes consistency in data collection, and facilitates effective communication among healthcare providers. The use of a wound assessment documentation template ultimately supports high-quality wound care and improved patient outcomes.
By utilizing a comprehensive wound assessment documentation template, healthcare providers can ensure thorough and consistent evaluation of wounds, leading to better treatment plans and improved patient outcomes. This ultimately allows for optimal wound healing and enhanced quality of life for individuals requiring wound care.