Hysteroscopy, a minimally invasive procedure that allows doctors to look inside the uterus, is becoming increasingly common. It’s used for everything from diagnosing the cause of abnormal bleeding to removing polyps or fibroids. However, like any medical procedure, accurate and comprehensive clinical documentation is absolutely crucial. It’s not just about ticking boxes; it’s about ensuring patient safety, facilitating effective communication among healthcare providers, and providing a clear legal record. Think of it as telling the patient’s story in a way that everyone involved in their care can understand.
So, why is having a solid clinical documentation template for hysteroscopy so important? Well, imagine a scenario where key details about a patient’s medical history or the specific findings during the procedure are missing. This could lead to misunderstandings, delays in treatment, or even potential errors. A well-designed template acts as a guide, ensuring that all essential information is captured consistently and accurately. This is not just a time saver; it’s a vital safety net for both the patient and the medical team.
In this article, we’ll delve into the essential elements of a good clinical documentation template for hysteroscopy. We’ll explore the key components you should include, discuss the benefits of using a standardized template, and offer practical tips for creating a template that works best for your practice. Consider this your comprehensive guide to creating effective and compliant documentation that will support the best possible patient care.
Why a Comprehensive Clinical Documentation Template Matters for Hysteroscopy
Clinical documentation is more than just paperwork; it’s the foundation of good medical practice. A well-structured template ensures that all critical aspects of the hysteroscopy procedure are documented, from the patient’s initial presentation to the post-operative follow-up. This includes details about the patient’s medical history, the indications for the procedure, the specific techniques used, and any complications encountered. Without this detailed information, it becomes difficult to provide consistent and effective care.
One of the primary benefits of using a standardized clinical documentation template for hysteroscopy is improved communication. When all members of the healthcare team have access to the same information, presented in a clear and organized manner, the risk of misunderstandings and errors is significantly reduced. This is particularly important in complex cases where multiple specialists may be involved. A well-documented record allows each provider to understand the patient’s condition and treatment plan, leading to better coordination of care.
Moreover, a comprehensive template helps to ensure legal compliance. Medical records are often used as evidence in legal proceedings, and a thorough and accurate record can protect healthcare providers from liability. A properly completed clinical documentation template for hysteroscopy demonstrates that the procedure was performed according to accepted standards of care and that all necessary precautions were taken. It also provides a clear audit trail, showing who performed the procedure, what was done, and why.
From a patient perspective, well-maintained clinical documentation contributes to a sense of trust and security. Patients want to know that their healthcare providers are paying attention to detail and that their medical information is being carefully managed. Clear and accurate documentation demonstrates a commitment to quality care and helps patients feel more confident in their treatment plan. This, in turn, can lead to better patient adherence and improved outcomes.
Think about the long-term benefits, too. Standardized documentation facilitates data collection and analysis, which can be used to improve clinical practice. By tracking outcomes and identifying trends, healthcare providers can refine their techniques and protocols, leading to better patient outcomes over time. In essence, a good template transforms documentation from a task into a valuable tool for continuous improvement.
Key Elements of a Clinical Documentation Template for Hysteroscopy
So, what should be included in a clinical documentation template for hysteroscopy? Here’s a breakdown of the essential components:
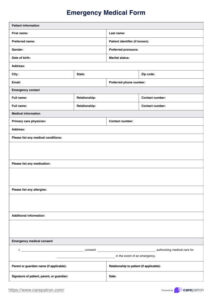
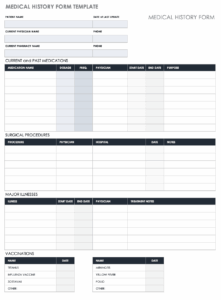
First, Patient Demographics and Medical History: This section should include the patient’s name, date of birth, medical record number, and contact information. Crucially, it should also include a detailed medical history, including any relevant past medical conditions, allergies, medications, and previous surgeries. Any risk factors, such as smoking or obesity, should also be noted here. This information provides context for the procedure and helps to identify potential complications.
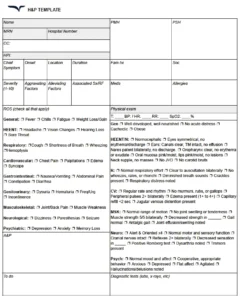
Second, Indications for Hysteroscopy: Clearly state the reason why the hysteroscopy is being performed. Is it for diagnosis of abnormal uterine bleeding? Evaluation of infertility? Removal of polyps or fibroids? Be specific and provide enough detail to justify the procedure. This section should also include the results of any pre-operative testing, such as ultrasound or endometrial biopsy.
Third, Procedure Details: This section should document the specifics of the hysteroscopy procedure itself. Include the date and time of the procedure, the type of anesthesia used, the instruments used, and any complications encountered. Describe the findings of the hysteroscopy in detail, including the size, location, and appearance of any abnormalities. If biopsies were taken, note the location and number of samples. Any interventions performed, such as polypectomy or myomectomy, should be documented here as well. Detailed drawings or images can be extremely helpful here.
Fourth, Post-Operative Instructions and Follow-Up: Provide clear instructions for the patient regarding post-operative care. This should include information about pain management, wound care, and any restrictions on activity. Schedule a follow-up appointment to assess the patient’s recovery and address any concerns. This section should also include contact information for the healthcare provider in case the patient experiences any problems after the procedure. Thorough post-op instructions can significantly reduce the risk of complications and improve patient satisfaction.
Finally, there should be a section for Complications and Adverse Events. No one wants to think about things going wrong, but it’s vital to document any complications or adverse events that occur during or after the procedure. This includes things like bleeding, infection, uterine perforation, or reactions to anesthesia. Document the details of the event, the steps taken to address it, and the patient’s response to treatment. Proper documentation of complications is essential for learning and improving patient care.
We’ve seen the positive impact of using good templates. A clinical documentation template for hysteroscopy is more than just a form to fill out; it’s a tool that supports patient safety, improves communication, ensures legal compliance, and facilitates continuous improvement in clinical practice.
By incorporating the key elements discussed in this article, you can create a comprehensive and effective documentation system that will benefit both your patients and your practice.