Critical care nursing is a high-stakes environment. Lives hang in the balance, and every second counts. In this fast-paced world, thorough and accurate documentation isn’t just a nice-to-have; it’s absolutely essential. Think of it as the lifeline of patient care, ensuring continuity, clarity, and ultimately, better outcomes. We all know that things get hectic in the ICU. Having a good system for recording what’s happening is crucial.
That’s where a well-designed critical care nursing documentation template comes into play. It’s more than just a form; it’s a tool that streamlines information gathering, promotes consistency, and helps nurses stay organized amidst the chaos. It ensures no critical detail is missed, providing a clear picture of the patient’s condition and the interventions being taken. Imagine trying to piece together a patient’s story from scattered notes and memory alone – a nightmare, right? A good template prevents that.
This article explores the importance of using a critical care nursing documentation template, highlighting the benefits it offers to both nurses and patients. We will dive into the key components of an effective template and discuss how it contributes to safer, more efficient, and more effective patient care. We will also touch on the role of technology and how it has impacted documentation practices in the ICU. So, let’s get started and explore how this valuable tool can make a real difference in critical care.
Why Accurate Documentation is Vital in Critical Care
In the critical care setting, documentation serves as the cornerstone of effective patient management. It’s the written record of everything that happens – every assessment, intervention, and observation. It’s not just about compliance, it’s about building a comprehensive narrative of the patient’s journey, informing clinical decisions, and ensuring seamless communication among the healthcare team. Without detailed and accurate records, we risk making critical errors, overlooking important information, and ultimately, compromising patient safety. Imagine a scenario where a subtle change in a patient’s condition goes unnoticed because it wasn’t properly documented. The consequences could be devastating.
Good documentation helps to improve communication between nurses, doctors, and other healthcare providers. Everyone needs to be on the same page. When information is clearly documented, it’s much easier for everyone to understand what’s going on and to make informed decisions about the patient’s care. This reduces the risk of misunderstandings and ensures that everyone is working towards the same goals. Think of it as creating a shared mental model of the patient’s condition.
Beyond communication, accurate documentation is crucial for legal and ethical reasons. In the unfortunate event of a medical complication or legal challenge, thorough and accurate records can provide essential evidence of the care provided. It demonstrates adherence to established protocols and standards of care, protecting both the nurse and the healthcare institution. Good documentation can also contribute to improved patient outcomes. By carefully tracking patient responses to interventions, nurses can identify trends and patterns that may not be immediately apparent. This information can be used to adjust treatment plans and improve the overall effectiveness of care.
Furthermore, documentation plays a key role in continuous quality improvement efforts. By analyzing documentation data, healthcare organizations can identify areas where processes can be improved and implement changes to enhance patient safety and efficiency. It provides a valuable source of information for audits, research, and performance evaluations. It also allows healthcare teams to learn from past experiences and to refine their practices over time. Ultimately, the goal is to create a culture of continuous learning and improvement.
To summarize, the importance of detailed documentation in a critical care setting is multifaceted, influencing patient safety, team communication, legal security, outcome improvement, and quality management. It is the foundation of good clinical practice. It should be prioritized and given sufficient resources to ensure that it is carried out to the highest standard.
Key Components of an Effective Critical Care Nursing Documentation Template
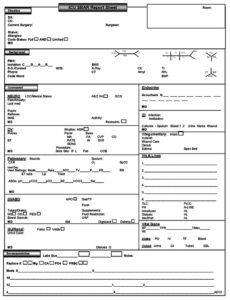
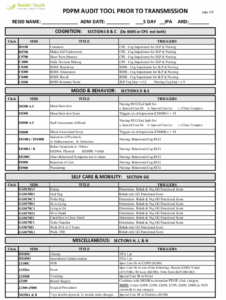
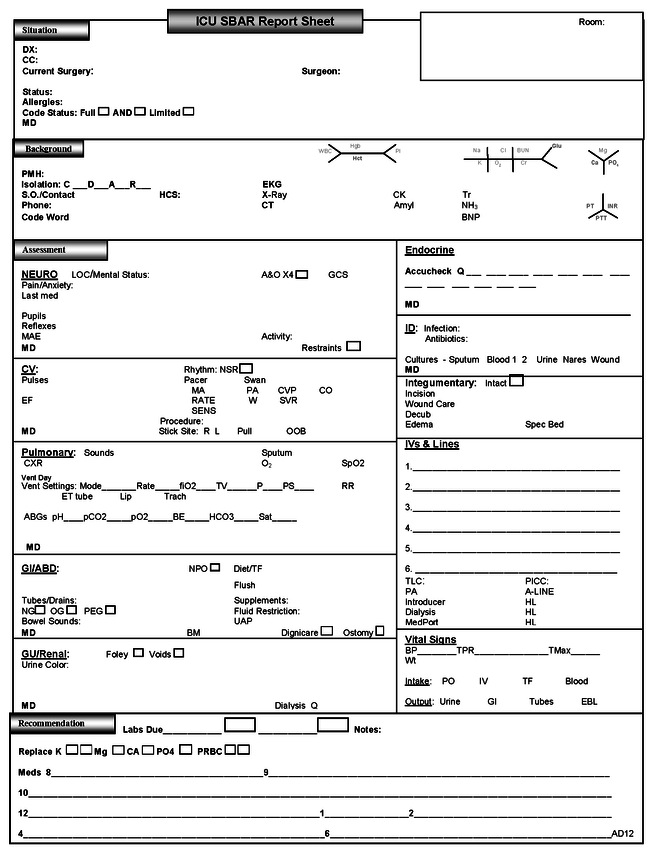
A well-designed critical care nursing documentation template should be comprehensive, easy to use, and tailored to the specific needs of the ICU. While the exact content may vary depending on the patient population and the institution’s policies, certain key components are essential. Let’s explore these components in detail.
First and foremost, the template should include a section for recording baseline patient information, such as demographics, medical history, allergies, and current medications. This information provides a foundation for understanding the patient’s overall health status and identifying potential risk factors. This section needs to be consistently updated to reflect any changes to the patient’s condition or treatment plan.
Next, the template needs to include a section for documenting vital signs, including heart rate, blood pressure, respiratory rate, temperature, and oxygen saturation. These measurements are crucial indicators of the patient’s physiological status and should be recorded frequently and accurately. The template should also include a space for documenting any interventions taken to address abnormal vital signs.
Neurological assessments are also critically important in critical care. The template should include a section for documenting level of consciousness, pupillary response, motor function, and sensory function. This information is essential for monitoring neurological status and detecting early signs of deterioration. It is essential to use a standardized assessment scale, such as the Glasgow Coma Scale (GCS), to ensure consistency and accuracy.
A comprehensive assessment of all body systems is crucial. The template should include sections for documenting respiratory status (breath sounds, oxygen requirements), cardiovascular status (heart sounds, edema), gastrointestinal status (bowel sounds, abdominal distension), and renal status (urine output, fluid balance). This comprehensive assessment allows nurses to identify potential problems and to initiate appropriate interventions. Consider adding a section for documenting pain levels and interventions related to pain management.
Finally, an effective critical care nursing documentation template should be easy to access, easy to use, and compliant with all relevant regulations and guidelines. Using a standardized template, perhaps one designed for a critical care nursing documentation template will also improve compliance and accuracy. It should also be regularly reviewed and updated to ensure that it remains relevant and effective. Ultimately, the goal is to create a tool that supports nurses in providing safe, efficient, and high-quality care to their patients.
Using the right documentation can make a world of difference. It’s about making sure that everyone on the healthcare team has access to the information they need to provide the best possible care. It’s also about protecting yourself and your colleagues by creating a clear record of the care that you’ve provided.
Think of this template as your partner in delivering great care. Embrace it, use it wisely, and let it help you make a real difference in the lives of your patients. When everything is clearly documented, things are done better.