Counseling is a deeply personal and impactful process, and behind every successful session lies meticulous documentation. Accurate and thorough records are more than just paperwork; they are the bedrock of ethical practice, legal protection, and effective treatment. Think of it as the counselor’s compass, guiding them through the client’s journey while ensuring accountability and continuity of care. It’s about capturing the essence of each interaction, the nuances of progress, and the roadmap for future interventions. In this article, we’ll explore the importance of documentation and how using a sound documentation in counseling records template can greatly enhance your practice.
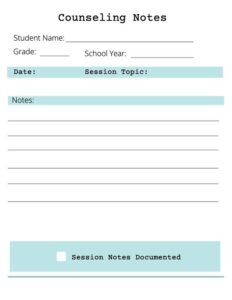
Navigating the world of counseling documentation can feel overwhelming at times. There are legal and ethical guidelines to consider, along with the practical need to create records that are both informative and efficient. Counselors often juggle demanding schedules, and finding the time to craft detailed notes after each session can seem daunting. That’s where a well-designed template comes in handy. It provides a structured framework, prompts you to include essential information, and ultimately streamlines the documentation process.
But it’s not just about saving time. Solid documentation provides invaluable insight into a client’s progress over time. It helps you track patterns, identify triggers, and tailor your approach to their specific needs. It can also be a crucial tool for supervision, consultation, and even legal defense if ever necessary. Good documentation is a reflection of good practice – demonstrating your commitment to client well-being and professional responsibility. So, let’s dive in and see how you can create a system that works for you.
Why Documentation in Counseling is Crucial
Documentation in counseling is far more than just a clerical task; it is a fundamental aspect of ethical and effective practice. It serves as a vital tool for tracking client progress, ensuring continuity of care, protecting both the client and the counselor, and upholding professional standards. Without proper documentation, counselors risk compromising the quality of their services and potentially facing legal or ethical repercussions. It’s the invisible thread that weaves together the tapestry of the therapeutic relationship.
One of the primary reasons documentation is crucial is that it provides a detailed record of the client’s journey. This record allows the counselor to track progress, identify patterns, and evaluate the effectiveness of interventions. By reviewing past notes, a counselor can gain valuable insights into the client’s evolving needs and adjust the treatment plan accordingly. This ensures that the client receives the most appropriate and effective care possible.
Furthermore, thorough documentation ensures continuity of care when a client transfers to another counselor or requires additional services. A comprehensive record provides the new counselor with a clear understanding of the client’s history, presenting problems, and treatment goals. This allows for a seamless transition and prevents the client from having to retell their story unnecessarily. It also helps avoid potential gaps in care that could arise from a lack of information.
Beyond its clinical benefits, documentation serves as a critical form of legal protection for both the client and the counselor. In the event of a complaint or legal action, accurate and detailed records can provide evidence of the services provided and the rationale behind treatment decisions. It demonstrates that the counselor acted ethically and responsibly, adhering to professional standards of care. This protection extends to the client as well, ensuring that their rights are upheld and that they receive fair treatment.
Finally, documentation is essential for meeting professional standards and ethical guidelines. Most professional counseling organizations have specific requirements for record-keeping, outlining the types of information that must be included and the length of time records must be retained. Adhering to these standards demonstrates a commitment to ethical practice and ensures accountability to the profession.
Elements of a Good Template
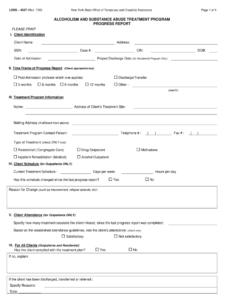
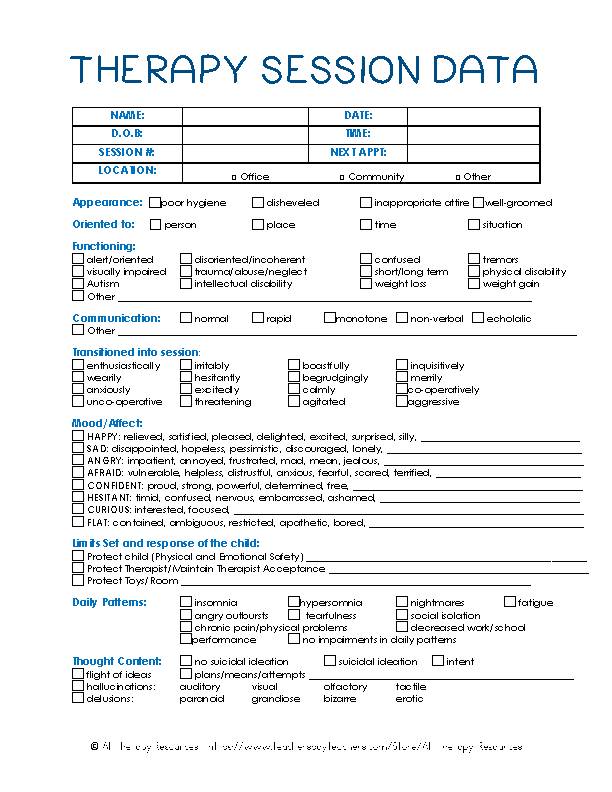
A robust documentation in counseling records template should include client demographics, presenting problems, treatment goals, interventions used, progress notes, assessment results, consent forms, and any relevant correspondence.
Key Components of an Effective Counseling Records Template
When designing or choosing a counseling records template, there are several key components to consider. These components ensure that the template is comprehensive, efficient, and compliant with ethical and legal requirements. A well-structured template will guide you through the documentation process, prompting you to include all the necessary information and reducing the risk of overlooking crucial details.
First and foremost, the template should include a section for basic client demographics, such as name, contact information, date of birth, and emergency contact details. This information is essential for identifying the client and ensuring that you can reach them or their emergency contact if needed. It also helps to maintain accurate records and avoid confusion with other clients.
The template should also include a section for recording the client’s presenting problem or reason for seeking counseling. This section should capture the client’s own words, as well as the counselor’s observations and assessment of the situation. It should also include any relevant history, such as previous diagnoses, medications, or significant life events. This information provides context for the client’s current struggles and helps to inform the treatment plan.
Another essential component of the template is a section for outlining treatment goals. These goals should be collaboratively developed with the client and should be specific, measurable, achievable, relevant, and time-bound (SMART). The treatment goals provide a clear direction for the counseling process and allow both the client and the counselor to track progress. The template should also include a space to document the interventions used to help the client achieve their goals.
Progress notes are a crucial part of the counseling record and should be included in the template. These notes should document the content of each session, including the client’s thoughts, feelings, and behaviors. They should also include the counselor’s observations, interventions, and any changes to the treatment plan. Progress notes should be written in a clear, concise, and objective manner, avoiding jargon or subjective opinions.
Finally, the template should include sections for documenting assessment results, consent forms, and any relevant correspondence. Assessment results, such as scores on standardized tests, can provide valuable information about the client’s strengths and weaknesses. Consent forms document that the client has been informed about the counseling process and has given their permission to participate. Any relevant correspondence, such as emails or letters, should also be included in the record to provide a complete picture of the client’s care.
The importance of maintaining accurate and complete documentation cannot be overstated. It’s an integral part of providing ethical and effective counseling services.
Using a reliable documentation in counseling records template helps streamline the process, ensuring that you capture all the essential information while saving valuable time.