Physical therapy practice thrives on clear, concise, and compliant documentation. It’s not just about ticking boxes; it’s about accurately reflecting the patient’s journey, the therapist’s expertise, and the rationale behind every treatment decision. Effective documentation protects both the patient and the practitioner, ensures continuity of care, and facilitates appropriate billing and reimbursement. Think of it as telling the story of your patient’s progress, a story that needs to be clear, accurate, and easily understood by anyone who reads it.
Finding the right documentation template can feel like searching for a needle in a haystack. There are countless options out there, each promising to simplify your workflow and improve your documentation practices. But what truly makes a template effective? It’s not just about aesthetics; it’s about functionality, compliance, and adaptability. A good template should streamline your process, prompt you to include essential information, and be flexible enough to accommodate the unique needs of each patient.
That’s where this guide comes in. We’re going to break down the essential elements of PT practice documentation, explore different template types, and provide practical tips for creating and using templates that work for you. This guide to pt practice documentation template will empower you to improve your documentation skills and choose the perfect template to enhance your practice.
Why Effective Documentation Matters in Physical Therapy
In the fast-paced world of physical therapy, documentation can sometimes feel like a burden. However, it’s far more than just paperwork. It’s the backbone of effective patient care, legal protection, and financial stability for your practice. Let’s dive into the core reasons why meticulous documentation is non-negotiable in the PT profession.
First and foremost, clear documentation ensures continuity of care. Imagine a patient who sees multiple therapists within a clinic or transitions to a home health setting. Comprehensive documentation allows each provider to understand the patient’s history, current status, goals, and treatment plan. This seamless transfer of information minimizes errors, avoids duplication of effort, and ultimately leads to better patient outcomes.
Secondly, proper documentation serves as a vital legal record. In the event of a lawsuit or audit, your documentation will be scrutinized to determine whether you provided reasonable and appropriate care. Detailed notes that accurately reflect your clinical reasoning, objective findings, and treatment interventions can protect you from liability and demonstrate your commitment to ethical practice.
Beyond legal considerations, accurate documentation is crucial for reimbursement. Insurance companies require detailed information to justify payment for services. Vague or incomplete notes can lead to denied claims, delayed payments, and lost revenue for your practice. By documenting thoroughly and accurately, you can ensure that you receive appropriate compensation for the services you provide.
Finally, strong documentation fosters communication within the healthcare team. It allows you to share important information with physicians, nurses, and other allied health professionals involved in the patient’s care. This collaborative approach promotes a holistic understanding of the patient’s needs and facilitates coordinated treatment planning.
Key Elements Of A Comprehensive Pt Documentation Template
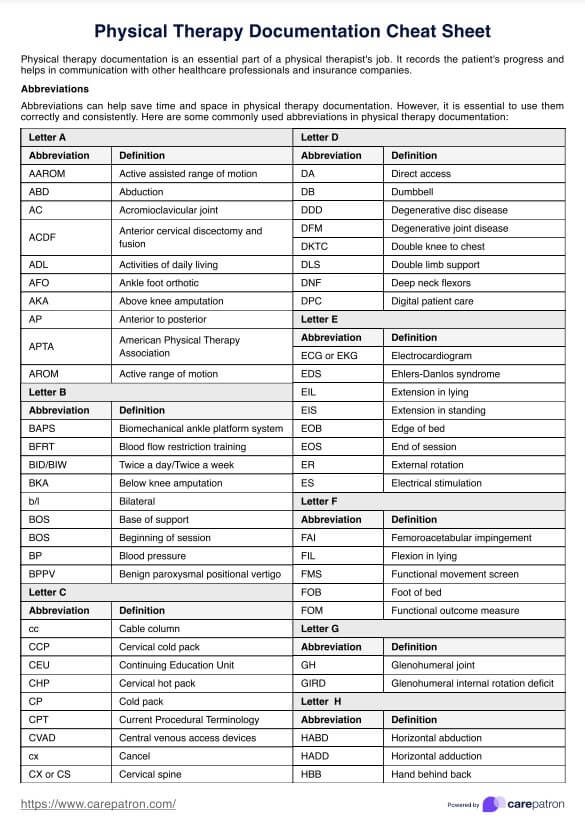
What makes a physical therapy documentation template truly comprehensive and effective? It’s more than just filling in the blanks; it’s about creating a framework that guides you to record all the essential information for each patient encounter. Here’s a breakdown of the key components you should look for in a template:
Patient Demographics and Medical History: This is the foundation of your documentation. Include the patient’s name, date of birth, contact information, relevant medical history, current medications, and any precautions or contraindications. This information is crucial for understanding the patient’s overall health status and tailoring your treatment plan accordingly.
Initial Evaluation: The initial evaluation is where you capture the patient’s chief complaint, history of present illness, functional limitations, and goals. It should include a thorough objective examination, including relevant tests and measures such as range of motion, strength, sensation, and balance. This forms the baseline against which you will measure progress throughout the course of treatment.
Treatment Plan: This section outlines your plan of care, including specific treatment goals, interventions, frequency, and duration. Goals should be SMART (Specific, Measurable, Achievable, Relevant, and Time-bound). Interventions should be clearly described, including modalities, exercises, manual therapy techniques, and patient education strategies.
Daily Treatment Notes: These notes document each treatment session, including the interventions performed, the patient’s response to treatment, any changes in their condition, and any modifications to the treatment plan. Be specific and objective in your descriptions, and avoid vague terms like “patient tolerated treatment well.” Instead, describe the patient’s performance, pain levels, and functional improvements.
Progress Notes: Progress notes are typically written at regular intervals (e.g., weekly or monthly) to summarize the patient’s progress towards their goals. They should include a review of the patient’s subjective complaints, objective findings, and functional abilities. Compare current status to the initial evaluation and identify any barriers to progress.
Discharge Summary: The discharge summary documents the patient’s final status, including their achieved goals, remaining limitations, and recommendations for continued care. It should include a summary of the treatment provided, the patient’s response to treatment, and any home exercise program or self-management strategies. This provides a valuable record for the patient and any future healthcare providers.
Documentation in physical therapy is a necessary task. Selecting a useful guide to pt practice documentation template is a great idea to improve patient care, protect your practice, and ensure appropriate reimbursement for your services. By investing in high-quality documentation practices, you can enhance the quality of care you provide and achieve better outcomes for your patients.