Dealing with abscesses and localized infections can be a common occurrence in various medical settings. When an incision and drainage procedure is necessary, proper documentation is crucial. Accurate and thorough records not only ensure quality patient care but also protect healthcare providers from potential legal issues. An incision and drainage documentation template serves as a guide to capture all relevant information during and after the procedure. This will help standardize the recording process, ensuring that nothing is missed.

The purpose of a well-structured documentation template is to create a clear, concise, and comprehensive account of the patient’s condition, the procedure performed, and the post-operative care provided. It helps maintain continuity of care, allowing other healthcare professionals to easily understand the patient’s history and treatment plan. Using a standardized template can improve efficiency and accuracy, minimizing errors and ensuring that all essential details are recorded.
In this article, we’ll explore the key elements of an effective incision and drainage documentation template, discuss the benefits of using one, and provide practical guidance on how to create or choose a template that meets your specific needs. We’ll also address the importance of proper documentation in mitigating risks and ensuring compliance with regulatory standards. Let’s dive into the world of effective documentation for incision and drainage procedures.
Key Elements of an Incision and Drainage Documentation Template
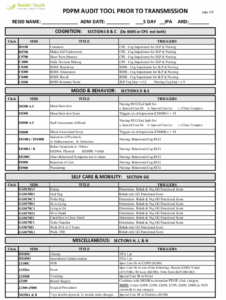
A comprehensive incision and drainage documentation template should include several key elements to ensure that all relevant information is captured. The patient’s demographic data, including name, date of birth, medical record number, and any relevant allergies or medical conditions, should be clearly recorded. The date and time of the procedure are essential for tracking the course of treatment.
Next, a detailed description of the abscess or infection site is necessary. This should include the location, size, shape, color, and any surrounding inflammation. Any relevant patient history that may have contributed to the infection, such as diabetes or immune deficiencies, should also be documented. Clearly documenting the pre-operative assessment is crucial for establishing a baseline and justifying the need for the procedure.
The procedure itself should be documented meticulously. This includes the type of anesthesia used (local, regional, or general), the instruments used, the incision technique, the amount and type of drainage obtained, and any complications encountered during the procedure. It is also important to note if any cultures were taken for further analysis. The wound should be assessed post-drainage, noting the appearance and any signs of bleeding or remaining infection.
Post-operative instructions and follow-up care are critical components of the documentation. These should include instructions on wound care, such as cleaning and dressing changes, as well as any medications prescribed, such as antibiotics or pain relievers. It’s important to clearly communicate the signs and symptoms of infection to watch out for, as well as contact information for the healthcare provider in case of concerns. Scheduled follow-up appointments should also be recorded to monitor the patient’s progress and ensure proper healing.
Finally, the documentation should include the healthcare provider’s signature and credentials, along with the date and time of the entry. This validates the accuracy and completeness of the record. Using a standardized incision and drainage documentation template helps ensure that all these key elements are consistently captured, promoting quality care and mitigating risks.
Benefits of Using a Standardized Incision and Drainage Documentation Template
Implementing a standardized incision and drainage documentation template offers numerous benefits for healthcare providers and their patients. One of the primary advantages is improved accuracy and completeness of records. A template provides a structured framework that prompts healthcare professionals to record all essential details, reducing the risk of omissions. This, in turn, leads to better-informed decision-making and enhanced patient care.
Efficiency is another significant benefit. A well-designed template streamlines the documentation process, saving time and effort for healthcare providers. Standardized fields and pre-defined options minimize the need for free-text entry, which can be time-consuming and prone to errors. This allows healthcare professionals to focus more on patient care and less on administrative tasks. This also allows other medical professionals to understand the patient history more efficiently if they are covering for the primary care provider.
Furthermore, a standardized template facilitates better communication and collaboration among healthcare providers. With consistent and easily accessible documentation, different members of the healthcare team can quickly understand the patient’s condition, the procedure performed, and the post-operative plan. This promotes continuity of care and reduces the risk of miscommunication or errors. It also becomes easier to share the documentation with other specialists if the patient requires follow-up care with a different provider.
Legal protection is another crucial benefit of using a standardized template. Accurate and thorough documentation serves as a legal record of the care provided, protecting healthcare providers from potential liability claims. In the event of a dispute or investigation, a well-documented record can provide evidence of appropriate care and adherence to standards of practice. An incision and drainage documentation template helps ensure that all relevant details are recorded, minimizing the risk of legal challenges.
Finally, using a standardized template supports quality improvement efforts. By collecting consistent data across all cases, healthcare providers can analyze trends, identify areas for improvement, and implement strategies to enhance patient outcomes. This data-driven approach helps drive continuous quality improvement and promotes best practices in incision and drainage procedures. Over time, analysis of documentation can lead to refinement of techniques and better overall patient care.
Healthcare professionals can ensure that their practices are well-organized, compliant, and focused on delivering the best possible care to their patients. It allows them to be more effective and confident in their skills.
Ultimately, the proper utilization of an incision and drainage documentation template ensures a high level of medical practice and legal compliance.