Navigating the world of healthcare often feels like wading through a sea of paperwork. Doctors, nurses, and other healthcare professionals are constantly documenting patient information to ensure continuity of care, accurate billing, and legal compliance. But let’s be honest, no one wants to spend more time filling out forms than they do actually caring for patients. That’s where a good medical documentation template history and physical comes in handy. It’s like a pre-designed roadmap that guides you through the necessary information to collect, saving you time and ensuring you don’t miss anything important.

Think of a medical documentation template history and physical as your trusty sidekick. It’s not meant to replace your clinical judgment or your ability to connect with your patients, but rather to streamline the process of capturing and organizing their story. A well-designed template will prompt you to ask the right questions, document the relevant findings from your physical exam, and formulate a clear and concise assessment and plan. This, in turn, improves communication among healthcare team members and leads to better patient outcomes.
In essence, using a structured medical documentation template history and physical is about working smarter, not harder. It helps you efficiently gather and record crucial patient data, freeing you up to focus on what truly matters: providing the best possible care. It also ensures that all the essential information is captured in a standardized format, which is vital for audits, legal protection, and overall quality assurance within the healthcare setting.
Benefits of Using a Medical Documentation Template History and Physical
The advantages of incorporating a medical documentation template history and physical into your practice are numerous. One of the most significant benefits is improved efficiency. Imagine spending less time wrestling with blank pages or trying to remember exactly what you need to document. A template provides a structured framework, guiding you through each section of the history and physical exam in a logical order. This reduces the risk of overlooking important details and ultimately saves you valuable time.
Beyond efficiency, templates enhance accuracy and completeness. They act as a checklist, reminding you of the key questions to ask and the specific elements to examine during the physical. By prompting you to document these details consistently, templates help to ensure that all relevant information is captured and recorded. This is particularly crucial in complex cases where a thorough and accurate record is essential for diagnosis and treatment planning.
Another key advantage is enhanced communication. When everyone uses the same template, the format and content of the documentation become standardized. This makes it easier for other healthcare providers to quickly review and understand a patient’s history and physical findings. Improved communication leads to better coordination of care and reduces the risk of errors or misunderstandings.
Furthermore, using a medical documentation template history and physical can help mitigate legal risks. A comprehensive and well-organized record provides evidence of the care provided and demonstrates that you met the required standard of care. This can be invaluable in the event of a malpractice claim or audit. The template prompts you to document all relevant information, ensuring that you have a complete and defensible record.
Finally, templates can contribute to improved patient satisfaction. When healthcare providers are more organized and efficient, patients feel more confident in the care they are receiving. A structured history and physical exam demonstrates that you are thorough and attentive to their needs. This can lead to increased patient trust and satisfaction, which are essential for building strong patient-provider relationships.
Types of Templates
There are many different types of medical documentation templates history and physical available, each designed to meet specific needs. Some templates are general in nature and can be used for a wide range of patients and conditions. Others are tailored to specific specialties, such as cardiology, pediatrics, or dermatology. Choosing the right template depends on your practice setting, patient population, and the types of conditions you commonly treat.
Some templates are paper-based, while others are electronic. Electronic templates offer the advantage of being easily integrated into electronic health record (EHR) systems, which can further streamline the documentation process. They also allow for easy searching and retrieval of information. Paper-based templates may be more suitable for settings where EHR systems are not available or where providers prefer to document by hand.
Key Components of a History and Physical Template
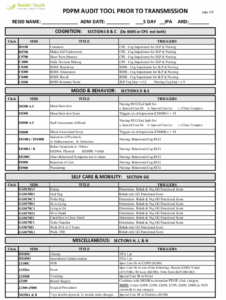
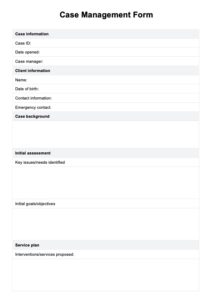
A comprehensive medical documentation template history and physical typically includes several key components, each designed to capture specific aspects of the patient’s health. The history section focuses on gathering information about the patient’s past and present medical conditions, as well as their family history and lifestyle factors. This section typically includes questions about the patient’s chief complaint, history of present illness, past medical history, surgical history, medications, allergies, family history, social history, and review of systems.
The physical exam section involves a systematic assessment of the patient’s physical condition, including vital signs, general appearance, and a head-to-toe examination of various organ systems. This section typically includes documentation of the patient’s blood pressure, heart rate, respiratory rate, temperature, and weight. It also includes a detailed examination of the head, eyes, ears, nose, throat, neck, chest, lungs, heart, abdomen, musculoskeletal system, neurological system, and skin.
The assessment section is where you synthesize the information gathered from the history and physical exam to formulate a diagnosis or differential diagnosis. This section should include a concise summary of the patient’s key findings and your interpretation of those findings. It should also include a discussion of any relevant medical literature or guidelines that support your assessment.
The plan section outlines your proposed course of action for managing the patient’s condition. This section should include specific recommendations for diagnostic testing, treatment, and follow-up. It should also include patient education and counseling regarding their condition and treatment plan. The plan should be tailored to the individual patient’s needs and preferences.
Finally, the template should include a section for documenting any relevant laboratory results, imaging studies, or other diagnostic tests. This section should include the date of the test, the results, and your interpretation of the results. It should also include any relevant consultations with other healthcare providers.
By meticulously recording all these details in the medical documentation template history and physical, healthcare professionals create a valuable record. This record serves as a guide for future care, facilitates communication between providers, and protects both the patient and the provider.
The responsible use of standardized forms improves quality of care. It also assures that patient stories are captured correctly and completely. This in turn benefits the patient and supports the physician in their work.