Navigating the world of nursing requires a multitude of skills, and one of the most crucial is the ability to accurately and comprehensively document patient assessments. Think of it as building a detailed narrative of a patient’s health status, a story that guides care and ensures continuity. That’s where a solid nursing assessment template for documentation comes in – it’s your organized roadmap through the complexities of patient information.
The goal isn’t just to fill in boxes; it’s about capturing a holistic view of the patient. It encompasses everything from their vital signs and medical history to their emotional state and social support system. Good documentation helps healthcare professionals communicate effectively, track changes in a patient’s condition, and make informed decisions regarding treatment plans. This is particularly important in today’s fast-paced healthcare environment.
Imagine trying to explain a patient’s condition to a colleague without clear, concise notes. It would be a frustrating and potentially dangerous situation! A well-designed template streamlines this process, making it easier to record information accurately and efficiently. Ultimately, effective nursing assessment documentation leads to better patient outcomes and improved quality of care.
Why is Accurate Nursing Assessment Documentation So Important?
Accurate nursing assessment documentation isn’t just about ticking boxes; it’s the cornerstone of safe and effective patient care. Consider it a legal document, a communication tool, and a crucial component of evidence-based practice, all rolled into one. Think of it like this: if you don’t document it, it didn’t happen. That statement might sound harsh, but it underscores the importance of thorough and meticulous record-keeping.
One of the primary reasons for detailed documentation is legal protection. In the event of a lawsuit or investigation, your notes serve as evidence of the care you provided. Clear, concise documentation demonstrates that you followed established protocols, made sound clinical judgments, and acted in the best interest of the patient. Ambiguous or incomplete notes, on the other hand, can leave you vulnerable to legal challenges.
Beyond legal protection, documentation facilitates seamless communication among healthcare professionals. Nurses, doctors, therapists, and other members of the care team rely on your notes to understand the patient’s condition, track their progress, and coordinate their efforts. When everyone is on the same page, the risk of errors and omissions is significantly reduced.
Furthermore, accurate assessment documentation plays a vital role in evidence-based practice. By meticulously recording patient data, you contribute to a growing body of knowledge that informs clinical decision-making. Analyzing patterns and trends in patient outcomes allows healthcare providers to identify best practices and improve the quality of care they deliver. It’s about using data to drive better results.
Think about the implications of poor documentation: delayed diagnoses, medication errors, ineffective treatments, and compromised patient safety. A seemingly small omission can have far-reaching consequences. Therefore, it is essential to prioritize accurate, comprehensive, and timely documentation in your nursing practice.
Key Elements of an Effective Nursing Assessment Template
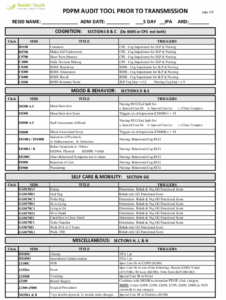
An effective nursing assessment template should be comprehensive yet user-friendly, guiding you through the essential components of a patient evaluation. It’s about striking a balance between thoroughness and efficiency, ensuring that you capture all the necessary information without becoming bogged down in unnecessary details. A good template acts as a roadmap, prompting you to ask the right questions and record the relevant findings.
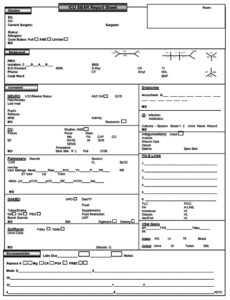
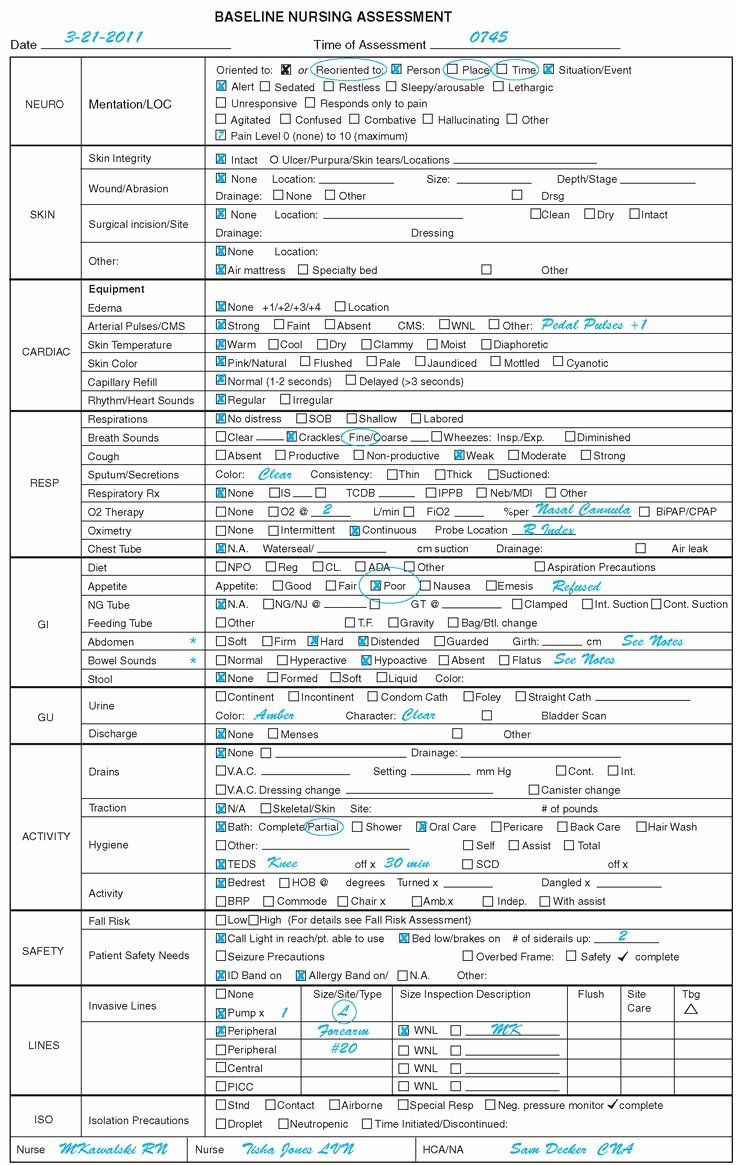
At its core, the template should include sections for demographic information, chief complaint, medical history, surgical history, medication list, allergies, and social history. These elements provide a foundational understanding of the patient’s background and potential risk factors. Be sure to include space for documenting the source of information (patient, family member, medical record) and the reliability of the source.
The physical assessment section is equally critical. This should cover all major body systems, including cardiovascular, respiratory, neurological, gastrointestinal, musculoskeletal, and integumentary. For each system, document your observations, palpations, auscultations, and any pertinent diagnostic findings. Use descriptive language to paint a clear picture of the patient’s condition, and avoid vague or subjective terms.
Don’t overlook the importance of documenting the patient’s psychosocial status. This includes their emotional state, cognitive function, support system, and coping mechanisms. Ask open-ended questions to elicit information about their concerns, anxieties, and goals for care. Documenting these aspects of the patient’s experience provides a more holistic understanding of their needs.
Finally, the template should include a section for nursing diagnoses, goals, interventions, and evaluation. Based on your assessment findings, identify the patient’s actual or potential problems and develop a plan of care to address them. Clearly articulate your goals for the patient, the specific interventions you will implement, and how you will evaluate the effectiveness of those interventions. This creates a clear framework for ongoing care and ensures accountability.
The nursing assessment template for documentation can be your best friend during a busy shift and will ensure all documentation aspects are covered.
We’ve explored the vital role of accurate nursing assessment documentation in ensuring safe and effective patient care. By implementing a well-designed template and prioritizing thoroughness, you can contribute to better communication, informed decision-making, and improved patient outcomes.