So, your shift is ending. You’ve been on your feet for hours, caring for patients, administering medications, and navigating the whirlwind that is a nursing shift. The last thing you probably want to do is spend more time writing notes. But accurate and thorough documentation is absolutely crucial in nursing. It’s not just about covering yourself; it’s about ensuring continuity of care for your patients and providing a clear picture of their status for the next shift. A well crafted nursing closing shift note for documentation template can save you time and headaches.
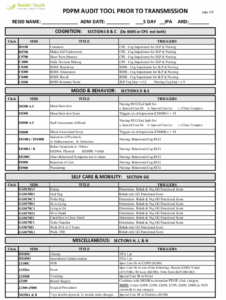
That’s where a good closing shift note for documentation template comes in handy. It acts like a structured guide, reminding you of the key elements to include and helping you organize your thoughts. Think of it as your secret weapon against end-of-shift fatigue and the urge to rush through documentation. It helps ensure important details don’t get missed in the handoff.
This article is designed to give you a comprehensive understanding of what constitutes a good nursing closing shift note and provide insights into creating or utilizing a template effectively. We’ll break down the essential components, offer practical tips, and discuss the importance of clear, concise, and accurate documentation. Let’s get started on making your end-of-shift routine a little less stressful and a lot more effective.
Crafting the Perfect Nursing Closing Shift Note: Essential Elements
A closing shift note is more than just a formality; it’s a vital communication tool that bridges the gap between nursing shifts. It provides the incoming nurse with a snapshot of the patient’s current condition, interventions performed during your shift, and any anticipated needs or concerns. A well-structured note helps to avoid misunderstandings and ensures that the patient receives consistent and high-quality care.
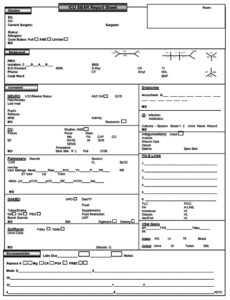
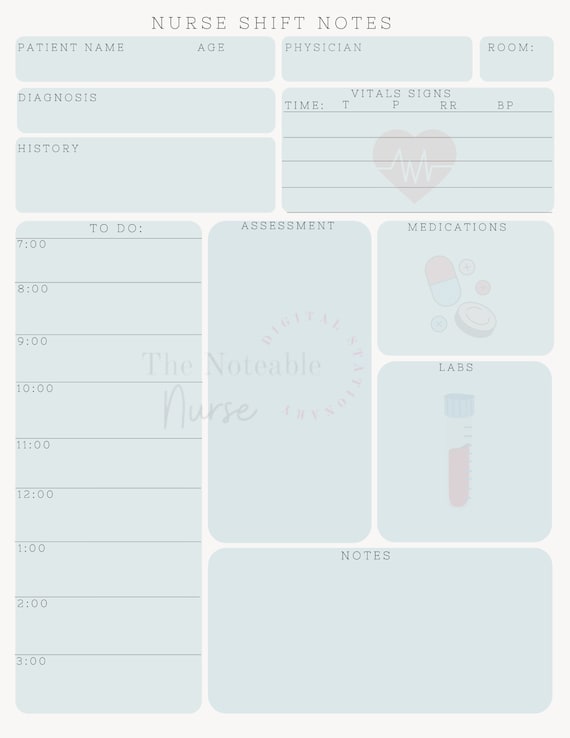
The specific information included in your closing shift note will vary depending on your unit, the patient’s condition, and hospital policies. However, there are some essential elements that should be included in almost every note. First and foremost, document the patient’s general condition. This includes their level of consciousness, vital signs, pain level, and any significant changes that occurred during your shift. Be specific and objective in your observations. Avoid vague statements like “patient seems tired.” Instead, document “patient reports fatigue; observed to be resting with eyes closed for extended periods.”
Next, clearly outline all the interventions you performed during your shift, including medication administration, wound care, respiratory treatments, and any other procedures. Include the time, dosage, route, and patient response for medications. If you encountered any difficulties or unusual circumstances during an intervention, be sure to document those as well. For example, “Medication X administered via IV at 10:00 AM. Patient tolerated medication without adverse effects. IV site assessed and found to be without signs of infiltration or infection.” Also, you should detail any communication with physicians, other healthcare professionals, or family members regarding the patient’s care. Include the date, time, and a summary of the conversation. This is especially important if there were any changes in the patient’s plan of care or if you received any new orders.
It’s also crucial to document any unresolved issues or potential problems that the oncoming nurse should be aware of. This could include pending lab results, equipment malfunctions, or patient concerns. For example, “Patient reports increased shortness of breath with exertion. Oxygen saturation remains at 92% on 2L nasal cannula. Physician notified; awaiting orders for further evaluation.” Don’t forget to document any patient education provided during your shift. This includes information about medications, treatments, or discharge instructions. Note the topics covered and the patient’s understanding of the information.
Utilizing a Nursing Closing Shift Note for Documentation Template Effectively
Using a template for your nursing closing shift note for documentation template can significantly improve efficiency and ensure consistency in your documentation. However, it’s important to use the template as a guide, not a replacement for your critical thinking skills. Don’t simply fill in the blanks without carefully considering the patient’s individual needs and circumstances.
Key Considerations for an Effective Closing Shift Note
Clarity and conciseness are paramount when writing closing shift notes. Use precise language and avoid jargon or abbreviations that may not be universally understood. Imagine someone unfamiliar with the patient reading your note – would they be able to understand the patient’s condition and the care provided? Always write legibly. If you are documenting electronically, ensure that your entries are clear and easy to read. If you have poor handwriting, make the effort to type or print clearly.
Accuracy is non-negotiable. Double-check your information, including medication dosages, vital signs, and lab results, before documenting them. If you make a mistake, correct it according to your facility’s policy. Never attempt to erase or cover up an error. Instead, draw a single line through the incorrect information, write “error” and your initials, and then document the correct information.
Patient confidentiality is of utmost importance. Never include any information in your notes that is not directly relevant to the patient’s care. Avoid using patient names or other identifying information in your notes if possible. It is important to remember that your closing shift note is a legal document. Be honest and objective in your documentation. Never falsify or alter information, even if you believe it will protect you or the patient. Accurate and truthful documentation is essential for providing safe and effective patient care, and it also protects you from potential legal liability.
Think about how your documentation could be interpreted if it were reviewed in a legal setting. Would it clearly and accurately reflect the care you provided? Would it demonstrate that you acted in the patient’s best interest? Taking the time to write a thorough and accurate closing shift note is an investment in both your patients’ well-being and your own professional security. Before you sign off on your shift, take a moment to review your notes and ensure that they are complete, accurate, and clear. This final check can help you catch any errors or omissions and ensure a smooth handoff to the next shift.
Effective documentation isn’t just about avoiding errors; it’s about proactive communication. By thoroughly documenting patient status, interventions, and any pertinent details, you’re setting the stage for the next nurse to provide seamless and informed care. This ultimately contributes to better patient outcomes and a more efficient healthcare environment.
Closing shift notes are a vital communication tool that helps to ensure that patients receive safe and effective care. It’s an essential part of the nurse’s role to diligently record every important detail.
By embracing the concepts and strategies discussed in this article, you can elevate your documentation practices and become a more effective and reliable member of the nursing team. Your commitment to clear, concise, and accurate closing shift notes will make a real difference in the lives of your patients.