Nursing documentation is the backbone of quality patient care. Think of it as the detailed story of a patient’s journey, recorded by the nurses who are closest to their needs. It’s more than just ticking boxes; it’s about capturing accurate, comprehensive, and timely information that informs decision-making, ensures continuity of care, and ultimately, protects both the patient and the healthcare provider. But how do you know if your nursing documentation is up to par? That’s where a nursing documentation audit template comes in.
A nursing documentation audit template provides a structured framework for reviewing patient charts and records to identify areas of strength and areas that need improvement. It helps ensure that documentation meets legal, ethical, and professional standards, as well as internal policies and procedures. It’s not about finding fault; it’s about fostering a culture of continuous improvement and enhancing the quality of care delivered.
Essentially, it’s a checklist on steroids. Instead of just vaguely hoping that everything is documented correctly, you have a systematic way to evaluate the completeness, accuracy, and legibility of nursing notes, medication administration records, care plans, and other essential documents. The process helps uncover inconsistencies, omissions, and potential risks, ultimately contributing to a safer and more effective healthcare environment. It’s a proactive step towards excellence in patient care.
Why Use a Nursing Documentation Audit Template?
There are several compelling reasons why incorporating a nursing documentation audit template into your workflow is a smart move. First and foremost, it improves patient safety. Accurate and complete documentation ensures that all members of the healthcare team have the information they need to make informed decisions about patient care. This reduces the risk of errors, omissions, and adverse events. Imagine a scenario where a patient’s allergy isn’t properly documented; the consequences could be life-threatening. Regular audits can help prevent such situations.
Secondly, a well-designed template promotes compliance with regulatory requirements and professional standards. Healthcare organizations are subject to numerous regulations regarding documentation, and failure to comply can result in fines, penalties, and even legal action. A nursing documentation audit template helps ensure that your documentation practices align with these requirements, protecting your organization from potential liabilities. For instance, The Joint Commission has specific standards related to documentation, and using a template can help you meet those expectations.
Thirdly, using a template enhances the efficiency and consistency of the documentation process. By providing a standardized format for reviewing records, a template streamlines the audit process and ensures that all areas are thoroughly assessed. This saves time and resources and reduces the potential for human error. When everyone is using the same tool and following the same process, it’s easier to compare results, identify trends, and implement targeted improvements.
Furthermore, an audit template can be a valuable tool for staff education and training. The audit process can identify areas where nurses may need additional training or support in documentation practices. This allows organizations to provide targeted education and improve the overall competence of their nursing staff. This could include training on specific documentation requirements, best practices for writing clear and concise notes, or the proper use of electronic health records.
Finally, regular audits contribute to a culture of continuous improvement. By identifying areas where documentation can be improved, healthcare organizations can implement strategies to enhance the quality of care and reduce risks. This is not about punishment; it’s about creating a learning environment where nurses are encouraged to reflect on their documentation practices and strive for excellence. It’s about fostering a proactive approach to quality improvement and ensuring that documentation is always up to par.
Key Components of an Effective Nursing Documentation Audit Template
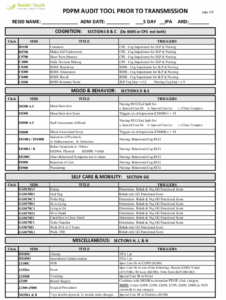
A good nursing documentation audit template shouldn’t just be a blank form; it should be a carefully structured tool that covers all the essential aspects of patient care documentation. The specific elements may vary depending on the setting and the organization’s needs, but some key components are universally important. First, it should address patient identification and demographics. This includes ensuring that patient names, medical record numbers, dates of birth, and other identifying information are accurately recorded on all documents. This is the foundation of accurate record-keeping, and any errors in this area can have serious consequences.
Secondly, the template should focus on the completeness of documentation. This means ensuring that all required elements of the record are present, such as nursing assessments, care plans, progress notes, medication administration records, and discharge summaries. The template should include specific criteria for evaluating whether each element is complete and contains all the necessary information. For example, a progress note should include the date, time, patient’s condition, interventions performed, and the nurse’s signature and credentials.
Thirdly, accuracy is paramount. The audit template should assess the accuracy of the information recorded, ensuring that it is factual, objective, and consistent with other sources of information. This includes verifying that medications are administered as prescribed, vital signs are recorded correctly, and patient symptoms and responses are accurately documented. Inaccurate documentation can lead to misunderstandings, errors in treatment, and potentially harmful outcomes for patients.
Fourthly, legibility is crucial, especially in paper-based records. The audit template should address the legibility of handwriting, ensuring that all entries are clear and easy to read. If documentation is illegible, it can be difficult or impossible for other healthcare providers to understand the information, leading to delays in treatment and potential errors. In electronic health records, legibility is less of a concern, but the template should still address the clarity and organization of the information.
Finally, the template should include a section for assessing compliance with legal, ethical, and professional standards. This includes ensuring that documentation is timely, confidential, and complies with all relevant regulations and policies. The template should also address issues such as informed consent, advance directives, and documentation of patient education. This component ensures that the documentation not only meets the needs of patient care but also protects the rights and privacy of patients.
Using a nursing documentation audit template doesn’t have to be an intimidating process. When done right, it serves as a valuable tool that elevates the standard of patient care. It’s a collaborative effort that empowers nurses to continuously improve their documentation practices. The aim is to create a safe and efficient healthcare environment for everyone.
Ultimately, the most successful healthcare providers are those who embrace proactive measures for continuous improvement. By incorporating a systematic nursing documentation audit template into your regular workflow, you are investing in the safety and well-being of your patients, protecting your organization from potential liabilities, and fostering a culture of excellence within your nursing staff.