Navigating the world of substance abuse counseling is a challenging but incredibly rewarding endeavor. You’re helping people reclaim their lives, build healthier futures, and find the strength within themselves to overcome addiction. But alongside the deeply personal work of therapy, there’s also the essential, and sometimes daunting, task of documentation. Let’s be honest, no one gets into this field because they love paperwork, but accurate and thorough documentation is crucial for ethical practice, legal compliance, and ensuring the best possible care for your clients. It can feel overwhelming, especially when you’re just starting out or trying to streamline your existing processes.
That’s where substance abuse counseling documentation forms template come into play. These templates aren’t just about ticking boxes; they’re about creating a structured framework for capturing vital information, tracking progress, and maintaining a clear record of your interactions with clients. Think of them as your trusted sidekick, helping you stay organized and focused on what truly matters: supporting your clients on their journey to recovery. Using a good template not only saves time but also helps ensure consistency and completeness in your records. This becomes particularly important when working within organizations that require adherence to specific standards and regulations.
In this article, we’ll delve into the world of substance abuse counseling documentation forms template, exploring why they’re so important, what types of forms are commonly used, and how you can choose or customize templates that best suit your practice’s needs. We’ll also touch on some best practices for using these templates effectively and efficiently, so you can spend less time wrestling with paperwork and more time making a real difference in the lives of those you serve.
Why Accurate Documentation is Essential in Substance Abuse Counseling
Accurate and comprehensive documentation isn’t just a “nice-to-have” in substance abuse counseling; it’s an absolute necessity. It forms the backbone of ethical, legal, and effective practice. Without proper documentation, you risk jeopardizing client care, exposing yourself to legal liabilities, and hindering your ability to track progress and make informed decisions.
Firstly, documentation plays a critical role in ensuring continuity of care. Clients may see multiple therapists, specialists, or healthcare providers throughout their recovery journey. Clear and detailed records allow these professionals to understand the client’s history, current needs, and past interventions, leading to more coordinated and effective treatment. Imagine a scenario where a client transfers to a new therapist without adequate documentation from their previous counselor. The new therapist would essentially be starting from scratch, potentially overlooking vital information that could impact the client’s treatment plan.
Secondly, documentation protects both the client and the counselor. In the event of legal or ethical challenges, thorough records can serve as evidence of the services provided, the rationale behind clinical decisions, and the steps taken to ensure client safety and well-being. It also provides a clear timeline of events and interactions, which can be crucial in defending against allegations of malpractice or misconduct. Good documentation demonstrates a commitment to ethical practice and adherence to professional standards.
Thirdly, proper documentation supports effective treatment planning and monitoring. By consistently recording observations, interventions, and client responses, you can track progress over time, identify patterns and trends, and adjust treatment plans accordingly. This data-driven approach allows for more informed decision-making and helps ensure that the client is receiving the most appropriate and effective care. Think of it as a roadmap guiding you and your client towards their recovery goals. Without a map, you’re essentially wandering aimlessly.
Finally, accurate documentation is often a requirement for reimbursement from insurance companies and other funding sources. Claims can be denied if documentation is incomplete, inaccurate, or fails to meet specific requirements. This can not only impact your revenue stream but also potentially jeopardize the client’s access to ongoing treatment. So, ensuring that your documentation is thorough and compliant is essential for maintaining financial stability and providing uninterrupted care.
Key Types of Substance Abuse Counseling Documentation Forms Template
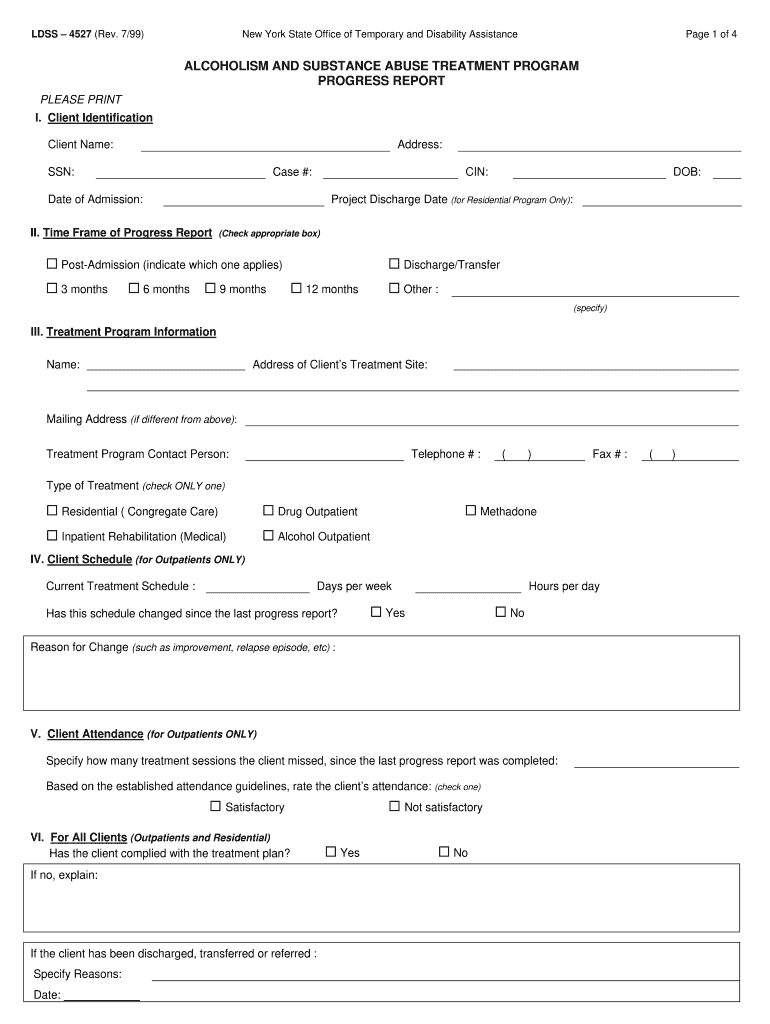
The specific types of documentation forms required in substance abuse counseling can vary depending on the setting, the client population, and applicable regulations. However, there are several core forms that are commonly used across most practices. Understanding these different types of forms and their purpose is essential for developing a comprehensive and efficient documentation system.
Intake Forms: These forms are typically completed at the client’s initial appointment and gather essential demographic information, medical history, substance use history, mental health history, and presenting problems. The intake form serves as a starting point for building a comprehensive understanding of the client’s background and needs. It helps you identify potential risk factors, assess the severity of the substance use disorder, and develop an initial treatment plan. A well-designed intake form should be clear, concise, and easy for the client to understand.
Assessment Forms: These forms are used to conduct a more in-depth evaluation of the client’s substance use disorder, mental health status, and overall functioning. They may include standardized questionnaires, such as the Addiction Severity Index (ASI) or the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria checklists. Assessment forms provide valuable data for diagnosis, treatment planning, and monitoring progress.
Treatment Plans: A treatment plan is a written document that outlines the client’s goals, objectives, and interventions for treatment. It should be developed collaboratively with the client and regularly reviewed and updated as needed. The treatment plan serves as a roadmap for therapy, guiding the counselor and client towards their desired outcomes. A well-written treatment plan should be specific, measurable, achievable, relevant, and time-bound (SMART).
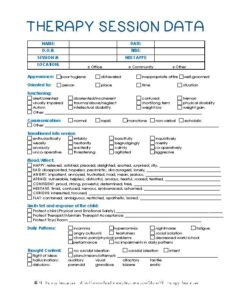
Progress Notes: Progress notes are brief summaries of each counseling session, documenting the date, time, and duration of the session, the topics discussed, the interventions used, and the client’s response. They should also include any significant observations or changes in the client’s condition. Progress notes are essential for tracking progress, monitoring treatment effectiveness, and providing evidence of services rendered. They should be written objectively and accurately, avoiding personal opinions or biases.
Discharge Summaries: A discharge summary is a comprehensive summary of the client’s treatment journey, including the reason for discharge, the goals achieved, the interventions used, and any recommendations for aftercare. It should be provided to the client and any other relevant healthcare providers upon discharge. The discharge summary serves as a record of the client’s treatment and a guide for continued care.
Implementing a system of substance abuse counseling documentation forms template can greatly improve the quality of care provided while streamlining the administrative work involved.
By keeping comprehensive notes, you ensure you’re not missing important details and can easily reference past sessions to inform current treatment strategies. It also aids in maintaining consistency and professionalism across your practice.